1. What Is Perioral Dermatitis?
If you’ve been diagnosed with Perioral Dermatitis, know that you are not alone—it is a condition we see and manage successfully very often. It’s a common and treatable inflammatory skin condition, and it’s important to know that it is not an infection and is distinct from acne, although it can sometimes look similar. It presents as a recognizable rash, most often on the face.


The condition typically looks and feels like a combination of the following characteristics:
- Appearance: The rash is usually made up of small inflammatory bumps (papules) and pus-filled spots (pustules), or it may appear as pink, scaly patches. The surrounding skin can often be dry, flaky, and scaly.
- Location: It most commonly appears around the mouth but can also develop around the nose (perinasal) and eyes (periocular).
- A “Clear Zone”: A key feature is often a clear, unaffected ring of skin directly bordering the lips.
- Sensations: Patients frequently report a burning sensation, a feeling of skin tightness, and sometimes itchiness in the affected areas.
While this rash is recognizable, understanding what might be causing or contributing to it can be complex.
2. Potential Causes and Contributing Factors
The exact cause of Perioral Dermatitis is unknown, and experts believe it is “multifactorial,” meaning several different factors can contribute to its development. Understanding these potential contributors can help you identify what might be triggering the condition in your own life.
Potential contributing factors include:
- Corticosteroid Use: This includes steroid creams applied to the skin as well as inhaled and nasal spray steroids.
- Cosmetics and Skincare Products: Certain ingredients or product types can trigger or worsen the rash.
- A weakened or damaged skin barrier: When the skin’s protective outer layer is compromised (for instance, due to very dry skin or harsh products), it can make you more susceptible to inflammation.
- Fluoride: This can be a factor whether it is in your toothpaste or water.
- Infectious Agents: In some cases, tiny organisms that live on the skin, such as mites or yeast, may play a role.
- Nutritional deficiencies: A lack of certain nutrients, like zinc, can sometimes be a factor.
- Other Factors: A variety of other elements have been linked to the condition, including chewing gum, hormonal changes, and environmental conditions like heat and wind.
Understanding these potential causes is the first step toward identifying specific triggers you may need to avoid.
3. Key Risk Factors and Triggers to Avoid
Identifying and avoiding personal risk factors is the most critical first step in managing Perioral Dermatitis and preventing future flare-ups. Below are the most well-known triggers to be aware of.
- Steroid Use This is the most common association with Perioral Dermatitis. The risk applies to steroids used in any form, including topical creams, inhaled medications for asthma, and nasal sprays for allergies. Chronic, long-term use of these products significantly increases the risk of developing a severe case.
- Certain Cosmetic Products Be particularly cautious with products that combine a moisturizer and a foundation. Heavy makeup and multiple layers can trap moisture and heat, creating an environment that irritates the skin and contributes to the rash.
- Fluorinated Dental Products For some individuals, fluoridated toothpaste is a clear trigger. Consider switching to a fluoride-free option during the healing process to see if it makes a difference.
- Heavy Skincare and a Weakened Skin Barrier Thick, heavy creams that block pores (occlusive products) can worsen the condition. Specifically avoid paraffin or petroleum-based creams. Similarly, a naturally weak or damaged skin barrier (e.g., very dry skin) increases your risk, as it’s less able to protect against irritants.
- Hormonal Changes Fluctuations in hormones can trigger the condition. This is why it is sometimes associated with the use of oral contraceptive pills, pregnancy, and premenstrual flares.
Recognizing these factors allows you to take targeted, actionable steps to help your skin begin to heal.
4. Your Action Plan: At-Home Management Strategies
While Perioral Dermatitis can be frustrating, there are several effective, non-prescription steps you can take immediately to calm your skin and encourage healing.
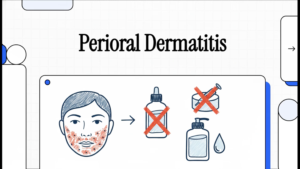
Adopt a “Zero-Therapy” Approach
This concept is simple but powerful: stop using all facial cosmetics, cleansers, and topical products on the affected areas. For mild cases of Perioral Dermatitis, this step alone may be enough for the rash to resolve over time. During this period, it is best to wash your face with only warm water.
Crucially, Stop All Steroid Creams
Discontinuing the use of any topical steroid creams is a primary recommendation.
Be prepared for a temporary flare-up. When you stop using a steroid cream, the rash may briefly get worse before it starts to get better. This is a common reaction, and it’s important not to restart the steroid.
In some cases, your doctor may recommend gradually reducing your use of the cream rather than stopping it abruptly to help minimize this flare.
Review and Simplify Your Products
Go through your daily routine and temporarily eliminate potential triggers. Create a “Stop Using” list that includes:
- Suspected cosmetics, especially combined foundations and moisturizers.
- Fluorinated toothpaste.
- Heavy, occlusive creams and ointments (like those based on petroleum or paraffin).
For Medically Necessary Steroids
If you use inhaled or oral steroids for a medical condition, do not stop taking them. However, you can help minimize their effect on your skin by rinsing your face and mouth with water after each use.
Commit to these changes for several weeks. While improvement is not immediate, giving your skin a complete break from potential triggers is the most powerful first step you can take toward healing.
5. What to Expect and When to See a Doctor
Managing Perioral Dermatitis requires patience, as it can be a stubborn condition. We understand that the visible nature of this rash can be frustrating and even cause emotional distress, which is why following a clear management plan is so important for both your skin and your well-being.
- Healing Takes Time: Be prepared for a gradual recovery. Improvement can take several weeks to months, even when you are carefully avoiding all known triggers.
- Recurrence is Possible: Perioral Dermatitis can be a chronic condition, meaning it may return. Recurrence is common, especially if triggers like corticosteroids are used again in the future.
- When At-Home Care Isn’t Enough: You should see a doctor if your condition is severe, does not improve after trying these at-home strategies, or if the initial flare-up after stopping steroids is too uncomfortable to manage. A doctor can confirm the diagnosis and offer effective prescription treatments to help clear the rash.
